Menstrual cramps are a fact of life for many women. Period cramps can range from slightly disruptive to indicative of a more serious condition that requires medical attention. But what causes menstrual cramps and how do you get rid of them fast? From changing your diet to quick-acting medications, there are many to cope with uterine pain, whenever you experience it.
Disclaimer: If you are worried about your health, please speak with your gynecologist. The following was written for informational purposes and is not medical advice.
4 Facts About Menstrual Cramps
New to the world of periods and not sure why your abdomen hurts? Literally billions of women have experienced period cramps before you. For the majority of us, experiencing abdominal pain once a month is a fact of life. To make this process less mysterious, here are a few things you should know:
- Over 80% of women experience menstrual cramps. They can affect their day-to-day work and school lives, according to research published in The British Medical Journal.
- 14% of women take time off of work or school as a result, according to the same study.
- The scientific term for this is dysmenorrhoea. Typically, it occurs within the days preceding menstruation. Usually, it manifests as pain in the lower abdomen.
- There are two kinds of dysmenorrhoea: primary and secondary. Primary is the most common: This is a natural pain that comes along with hormone fluctuations during and before menstruation. Secondary dysmenorrhoea is symptomatic of a larger health issue such as endometriosis or adenomyosis. If you are concerned that you are experiencing either of these conditions, please contact a physician.
We are not doctors. The following information is intended for educational purposes. If you have any specific medical questions, please contact your physician to learn more about what causes menstrual cramps, how to prevent them, and more.
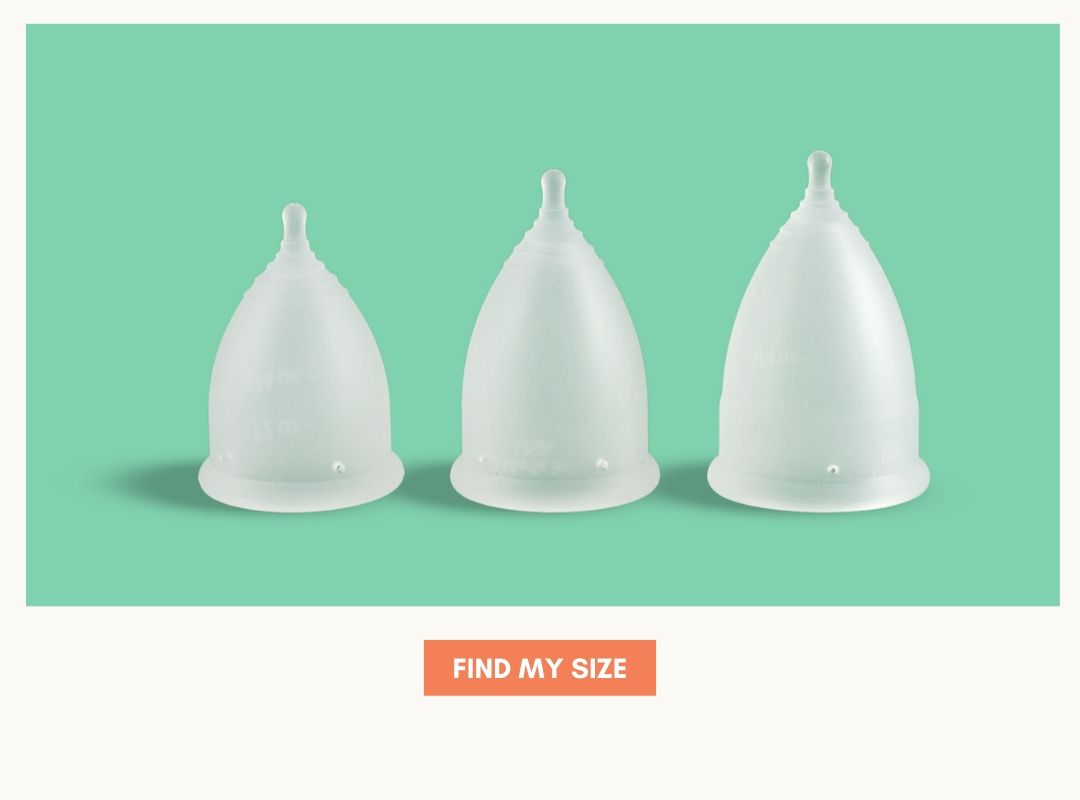
Check Out the EverCup Trio: Include 3 Different Sizes.
What Causes Menstrual Cramps?
Women have experienced periods and PMS symptoms for as long as we can remember. But while we're clutching a pint of Ben and Jerry’s in bed and holding a hot pack to our stomachs, what's the best way to deal with the pain? To understand period cramps, it’s essential to know a little about the menstrual cycle and why you would be experiencing any pain at all.
Understanding Your Cycle
A healthy part of a woman’s cycle is the shedding of the uterine lining, also called the endometrium. This—combined with the non-fertilized eggs—is released in the form of what we call a period. In order for the body to do this, the endometrium releases hormones called prostaglandins.
Prostaglandins serve a key function: They let the uterus relax and contract so that the lining can be released. With the perfect amount of prostaglandins, the body would not experience any pain. However, too much of these hormones may cause reduced blood flow, strong contractions, and a decrease in oxygen. These processes manifest as the menstrual cramps you dread every cycle. In other words, this pain is just a type of uterus-specific inflammation.
What Percentage of Women Experience It?
Depending on your data source, between 70% and over 80% of women experience mild to severe menstrual cramps. One study published in the Journal of Women’s Health that considers global figures found that 71% of menstruating women under 25 experience them. That's a lot of people.
It’s common for women to begin noticing pain after 6 months of menstruation, according to a study on primary and secondary dysmenorrhoea. This phase is called menarche. And as a woman’s cycle becomes more regular, so does the pain that comes along with it.
When Do Period Cramps Occur?
Though pain is not universal, research put forth in Informed Health states that most women experience menstrual cramps immediately preceding or at the time of bleeding. Typically, the pain lasts between one and three days and symptoms can range from mild to severe.
The same study found that 10% of women report pain that affects their daily life for up to three days of each cycle. Pain is most common in women under 20 years old. It is common for period cramps to lessen with age or following the birth of a child.
How to Get Rid of Period Cramps in 7 Ways
There are many ways to cope with your cycle, ranging from medications to self-care routines. If your cycle is extremely painful, the best thing to do is to contact your gynecologist. In some cases, they will prescribe hormonal birth control or another type of medication.
Beyond that, knowing how to get rid of menstrual cramps usually comes down to finding a healthy and effective way to reduce inflammation. This may mean testing out the following, which we’ll explore these in detail later on.
- Anti-inflammatory painkillers: Ibuprofen and Midol are common anti-inflammatory medications that some women use to control pain.
- Hormonal birth control: The hormonal IUD or the pill are often prescribed to cope with long-term and severe symptoms.
- Sex: Orgasms may reduce pain, giving you another great reason to enjoy period sex.
- Diet: Certain diets that can reduce inflammation may also help reduce period cramps. Additionally, adding specific vitamins and minerals may aid with pain management.
- Working Out: Exercise may also reduce pain and inflammation.
- Heat and Gentle Pressure: A heating pad or pillow is a tried and true method to get rid of menstrual cramps fast.
- Self Care: Your body and mind are linked in ways we're just starting to understand. Relieving stress may help cope with pain, too.
How to Get Rid of Menstrual Cramps Fast: Ibuprofen and Midol
Is the pain creeping up on your way to work? You don’t have time for a run or change your diet, so the best course of action may be an over-the-counter anti-inflammatory painkiller. These are called NSAIDs, which stands for non-steroidal anti-inflammatory drugs.
Why would Ibuprofen help with period cramps? By definition, it reduces inflammation. According to a University of Auckland study, NSAIDs were an effective way to treat primary dysmenorrhoea—the type that does not suggest an underlying medical condition—though women should be aware that NSAIDs may produce negative effects, such as gastrointestinal effects.
Please speak with a doctor is you are considering making NSAIDS part of your monthly pain management routine.
Using Hormonal Birth Control
By definition, hormonal birth control can prevent ovulation. If the uterine lining is not shedding, then a woman may not experience the pain associated with this process. The connection between severe menstrual cramps and birth control is explored more in-depth in a Journal of Women’s Health study.
Choosing the right type for your body is a decision you should make with medical experts. To learn more about whether hormonal birth control is right for you, please speak with your gynecologist.
Sex for Period Cramps
You heard right: Having an orgasm may be your answer to how to get rid of period cramps. This is because orgasms may dull pain, according to research published in The Atlantic. Of course, only do what is comfortable for your body.
Diet, Vitamins, and Nutrition
We’re just starting to understand the relationship between diet and what causes menstrual cramps. Here’s what some research has demonstrated thus far:
Women with a healthy, balanced diet are less likely to experience severe symptoms. Specifically, one study found that subjects whose diets consisted of “sugars, salty snacks, sweets and desserts, tea and coffee, salt, fruit juices and added fat” had a higher chance of experiencing more severe primary dysmenorrhea.
This was in comparison to women who adhered to a vegetarian diet and those who followed a “Mixed Food Items” diet, which included red meat, fast food, chicken, eggs and more.
A Close Look at Vitamins and Minerals:
- Magnesium deficit could contribute to dysmenorrhoea, according to a larger report published in The Journal of Clinical Endocrinology & Metabolism.
- Ginger may reduce symptoms according to one study comparing the effects of ginger capsules and ibuprofen published in 2009.
- Significant research shows that Zinc may help. To learn more, check out peer-reviewed medical journal Medical Hypotheses.
- Vitamins B1 and B6 may also reduce period cramps (see the study “Herbal and dietary therapies for primary and secondary dysmenorrhoea,” which also found magnesium to be an effective supplement).
Working Out to Reduce Menstrual Cramps
Another natural way to improve the symptoms that come along with your menstrual cycle is working out. As one study explains it, “Clinicians can inform women that physical activity may be an effective treatment for primary dysmenorrhea.” Keep in mind that this research looked exclusively at primary dysmenorrhea, rather than secondary dysmenorrhoea, which may indicate endometriosis or adenomyosis and requires medical attention.
Heat: An Ancient Remedy
Women have been using heat to reduce menstrual cramps for centuries history. In fact, heat may be equally effective as medications such as NSAIDs according to research published in Scientific Reports. Knowing how to get rid of period cramps may be as simple as using a heated water bottle or heating pad.
Self Care
Stress has real physical consequences—one of which is causing pain during your cycle. More scientifically, one study found that the risk of primary dysmenorrhea was twice as high among women under stress and with a family history of symptoms.
Concerned about period cramps? Taking the time for #selfcare may help reduce your pain when Aunt Flo comes around. This can mean taking a bath, practicing yoga or meditation, or doing anything that helps you relax after a long day.
7 Ways to Get Rid of Menstrual Cramps
Wondering how to get rid of period cramps? Every woman develops her own ritual to cope with the pain that may come along with a healthy cycle. For some, an anti-inflammatory may do the trick while other women benefit from adopting a more balanced diet and stress-free lifestyle.
Experiencing severe menstrual cramps? Remember that there are two types of dysmenorrhea: primary and secondary. If you have any questions or concerns regarding secondary dysmenorrhea please speak with a gynecologist. The above is not medical advice, nor should it be treated as such.